Fertility updates: The 2016 guide
Want children? Trying? Or maybe you’re just not sure? Charlotte Haigh MacNeil answers all your FAQs and gives you the most up-to-date options for starting a family

The most up-to-date options for starting a family whether you are trying right now, or simply want to be informed for the future...
Want children? Trying? Or maybe you’re just not sure? Charlotte Haigh MacNeil answers all your FAQs and gives you the most up-to-date options for starting a family
I’m not sure if I want children. Should I freeze my eggs just in case?
It could be ‘a good insurance policy,’ asserts Dr Amin Gorgy, co-director of The Fertility & Gynaecology Academy in London, who recommends doing it before the age of 37. ’After that, the quality isn’t like to be good enough,’ he says. ‘Poor-quality eggs are less likely to develop, which is why it can be harder to conceive when older. If you’re using eggs frozen when you were younger, your chances are much better.’
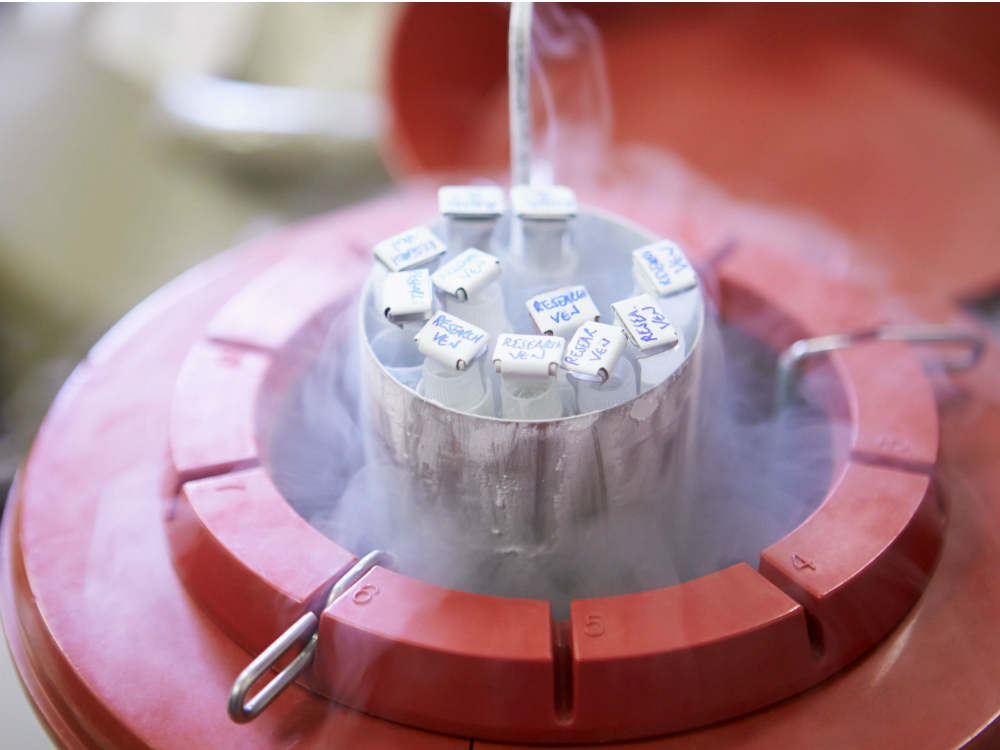
While it once had a reputation for being unreliable, these days, about 90 per cent of eggs survive thanks to ‘vitrification’, the latest technology that avoids the formation of ice crystals during the freezing process. But there are still no guarantees. ‘If a woman under 35 freezes about 12 eggs, she could have up to a 50 per cent chance of success later,’ says De Geeta Nargund, medical director of Create Fetility.
A cycle of egg-freezing can cost up to £5000, and involvesa needle through your vagina to take out the eggs. Mature eggs are stored at a clinic (costing £200 to £300 a year) until you are ready.
If I’ve had an abortion or miscarriage in the past, will that affect my chances of getting pregnant?
Marie Claire Newsletter
Celebrity news, beauty, fashion advice, and fascinating features, delivered straight to your inbox!
Good news – this is very unlikely. ‘Women worry about a condition called Asherman’s syndrome, caused by scar tissue developing in the uterus after a termination,’ says Tim Child, medical director of Oxford Fertility. ‘This can make it difficult for a pregnancy to implant. But Asherman’s is very rare. If anything, a previous pregnancy is usually a reassuring sign you’re fertile.’ About one in four pregnancies ends in miscarriage. This is mainly down to abnormal chromosomes in the baby. Most women go on to have a healthy pregnancy. Should we be ‘saving’ the sperm for my fertile days?
‘If a man ejaculates only every two or three days, the number of sperm is higher. If you have sex every day, there are fewer sperm per ejaculation but their motility is better,’ says Child. ‘So it’s swings and roundabouts. Sperm lives in your body for two or three days and the egg lives for a couple of days after ovulation, so the National Institute for Health and Care Excellence guidelines on fertility advise having sex every two or three days throughout your cycle.
You’ll ovulate around 14 days before your period, but I don’t advise timing sex to coincide with ovulation. Some research shows that couples waiting for the right time risk missing ovulation, plus it puts a lot of pressure on you both.’
What’s the latest research in infertility treatment?
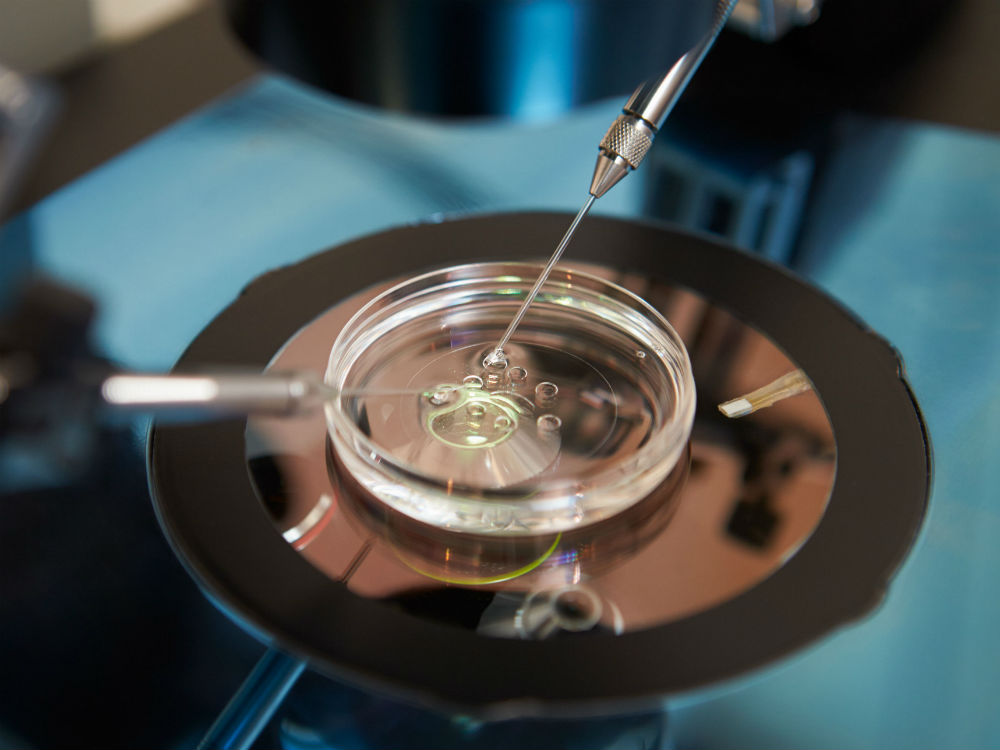
New developments are all about boosting live birth rates. ‘All women produce embryos with chromosomal abnormalities, which may fail to implant or miscarry,’ says Dr Gorgy. ‘Clinics can now perform pre-implantation genetic screening (PGS) of fertilised embryos before they’re put in the womb. We can exclude embryos with extra or missing chromosomes and those that carry defects. An immune system imbalance can play a role in fertility problems,’ he explains.
‘For instance, some women have too many natural killer (NK) cells in the lining of the uterus. These are immune system cells that fight off infections, but if your levels are too high they may attack a foetus. About 20 per cent with unexplained infertility going through IVF have immune issues. We treat them with medicine to suppress the overactive cells.’ Can fertility treatment give you cancer?
‘Good studies have found IVF doesn’t lead to an increased risk in any female cancer,’ says Nick Raine-Fenning, associate professor in reproductive medicine and surgery at the University of Nottingham. ‘Some research showed multiple IVF cycles in women under 25 could raise the risk of ovarian cancer.
There is a possible increased risk of ovarian cancer in women who take Clomid – given to stimulate ovulation – for more than a year. But it’s a small risk and most women wouldn’t take it for that long.’
I want to get pregnant. What can my partner and I do to increase our chances?
If either of you smokes, quit. Smoking can damage sperm and bring on menopause a few years early. But the jury is still out on e-cigarettes. ‘We don’t really know about their long-term effects or safety,’ says Raine-Fenning. ‘But if you’re using them to help you quit, anything has to be better than smoking.
However, it’s best if you’re neither smoking nor using e-cigarettes – the ovary of a smoker actually looks older.’ Improving nutrition, with a diet of plentyof fresh fruit and vegetable high in antioxidants, can help both partners.
‘For men, just two or three months of having a healthy lifestyle can make a big difference to abnormal sperm,’ says Raine-Fenning. You don’t have to go all Gwyneth, though, ‘With alcohol and caffeine, lower levels are better, but there’s no need to cut them out completely,’ says Child. ‘One glass of wine a night is fine.’
Start taking folic acid to reduce the risk of neural tube defects in a baby, and a general pre-conception multivitamin can be a good back-up. But while the fertility forums buzz with stories of supplements that can help improve egg quality over 35, in most cases the science isn’t strong, says Raine-Fenning. ‘However, there’s evidence that a supplement called DHEA may help some women.’
We’ve all heard stories of stressed-out couples who conceive when they take a holiday, but only extreme stress affects ovulation. ‘With lower stress levels, the picture is less clear,’ he adds. ‘I was involved in a study that found levels of the stress hormone cortisol were high throughout IVF, but it didn’t affect the outcome. That said, if you’re trying to conceive naturally, stress may influence cycles. So it is worth taking steps to reduce it.’ Just how difficult is it to get pregnant if you’re over 35?
‘Your fertility doesn’t fall off a cliff, but it does begin to drift downwards,’ says Raine-Fenning. ‘There’s typically another drop at 38, then it speeds up more at 40.’ This doesn’t mean you can’t get pregnant when you’re older – the number of eggs you have left in your ovaries falls at different rates from woman to woman.
If you want to predict your future, you could have a fertility MOT at a private clinic, with tests including an Anti-Mullerian Hormone (AMH) test, which can tell doctors how many eggs you’re releasing. ‘But the tests don’t tell us about egg quality, and that’s often what causes problems over 35,’ he says. ‘You could have good ovarian reserve but still struggle to get pregnant.
Conversely, poor results don’t mean you can’s conceive if you’re still ovulating every month, and plenty of women get pregnant easily without even knowing if they have low ovarian reserve. But if you’re worried, the tests could be useful. Have your tubes and uterus checked, too. If you have any issues, such as endometriosis, fibroids or ovarian cysts, it’s best to get them addressed now.’
I don’t have a partner. What are my options?
In Denmark, one in ten babies conceived with donor sperm is born to a single woman, and elective single motherhood is on the rise in the UK, too. You’ll have to fund it yourself, though. ‘Treatment with donor sperm isn’t generally available to single women on the NHS, as to qualify you have to have a medical condition that prevents you from conceiving,’ says Child. ‘But you could have donor insemination or IVF at a private clinic.’
Aside from chancing it and hoping the right relationship will happen, you could freeze your eggs [see previous page]. The price of a semen sample varies, but it may be up to £500 for a single sample – that’s enough for just one attempt. You then have the cost of intrauterine insemination (where the sperm is inserted around the time you ovulate) – which totals about £800 – or IVF (with drugs given to stimulate the ovaries to produce lots of eggs), which costs upwards of £3,500.
The leading destination for fashion, beauty, shopping and finger-on-the-pulse views on the latest issues. Marie Claire's travel content helps you delight in discovering new destinations around the globe, offering a unique – and sometimes unchartered – travel experience. From new hotel openings to the destinations tipped to take over our travel calendars, this iconic name has it covered.
-
 Style Briefing: Matthieu Blazy's last hurrah at Bottega Veneta
Style Briefing: Matthieu Blazy's last hurrah at Bottega VenetaHow the designer delivered a fresh perspective while also honouring its history of craft and creativity
By Rebecca Jane Hill
-
 The Emily in Paris cast has spoken out as one of its stars officially quits the show
The Emily in Paris cast has spoken out as one of its stars officially quits the showBy Jenny Proudfoot
-
 Timothée Chalamet’s mother has opened up about his relationship with Kylie Jenner
Timothée Chalamet’s mother has opened up about his relationship with Kylie JennerBy Jenny Proudfoot